CalPERS Driving Improvements in Healthcare: The Quality Alignment Measure Set and Incentives
June 2024
CalPERS has established quality performance measures that tie substantial financial incentives for the health maintenance organizations (HMOs) it contracts with to improve the quality of healthcare, and to eliminate health disparities for CalPERS members and all Californians. Specifically, the Quality Alignment Measure Set (QAMS) and their related financial incentives focus on improving care for a few clinically important conditions for which there are major opportunities for improvement and evidence-based measures in current use.
The QAMS and incentive structure were adopted for CalPERS HMOs in 2024, with the first potential payment due for not meeting targets payable for plan year 2025. With its new preferred provider organization (PPO) contract for 2025 through 2029, CalPERS has aligned with the quality measures and financial incentives already in place in the HMO contracts for 2024. Our goal with these substantial guarantees around quality is to have CalPERS PPOs be as quality- and equity- centered as our HMOs, so that we have the same high quality and equity standards for all our CalPERS Basic members, regardless of whether they are in an HMO or PPO.
The information in this fact sheet illustrates the focus on quality in CalPERS HMO and PPO plans, as well as its potential impact on improving care for all Californians. The details on the financial incentives can be found on CalPERS’ New Total Cost of Care Guarantee Terms in PPO Contracts Aligns Incentives to Lower Health Care Trend.
Quality Alignment Measure Set (QAMS)
The QAMS consists of five measures, all of which are nationally endorsed, evidence-based National Committee for Quality Assurance (NCQA) Healthcare Effectiveness and Data Information Set (HEDIS) measures:
- Childhood Immunizations
- Controlling High Blood Pressure
- Comprehensive Diabetes Care – Poor Control (HgbA1c >9%)
- Colorectal Cancer Screening
- Maternity Care – reflecting a combined score for:
- Timeliness of Prenatal Care
- Postpartum Care
In addition to the QAMS, all of CalPERS HMOs and its PPO plan will report on the following NCQA HEDIS measures for each of its products: Depression Screening and Follow-Up for Adolescents and Adults (DSF) and Pharmacotherapy for Opioid Use Disorder (POD). CalPERS is considering including these measures in the QAMS after benchmarks have been established.
As part of its commitment to addressing health equity, CalPERS requires plans to break down and report the QAMS by race and ethnicity to assess disparities and then develop disparity elimination plans. CalPERS is also working with Covered California, the Department of Health Care Services (DHCS) and the Department of Managed Health Care (DMHC) to develop a methodology to develop performance targets tied to financial incentives for eliminating disparities related to the QAMS.
Benchmarks and Financial Incentives for Higher Quality
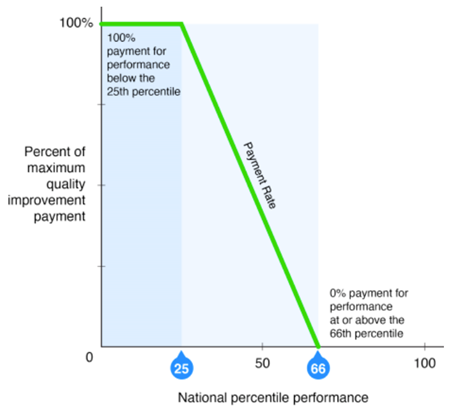
CalPERS is utilizing the same measures and the same benchmark – the NCQA-derived national 66th percentile – for both its HMOs and its PPO plan, with the same incentive structure. Specifically, for each measure with a result below the benchmark (66th percentile), the PPO plans, administered by both the third-party administrator (TPA) and the population health management (PHM) vendor, must each make a payment as outlined below (see Figure 1. CalPERS QAMS Quality Improvement Payment Structure):
- Below 25th percentile: full payment for each measure result
- At or above the 25th to the 65th percentile: payment per measure is assessed proportional to position in that range (sliding scale – meaning, the amount increases the closer it is to the 25th percentile).
- At or above 66th percentile: no measure payment
Quality Aligned Financial Incentives for CalPERS HMOs
For CalPERS HMOs, issuers that fail to meet the specified measure benchmarks will be required to make payments to CalPERS. For Plan Year 2024 (which is also the year from which results are derived), 1% of each HMO’s total gross premium per product is at risk for performance on the QAMS. The total amount at risk for the QAMS will increase to 2% of total gross premium per product in Plan Year 2025, increasing by 1% per year up to 4% in 2027.
Quality Aligned Financial Incentives for CalPERS PPO and Population Health Management Firm
For its self-funded PPO program, the TPA is responsible for reporting on the QAMS and both the TPA and the PHM vendor share financial accountability for the measure results. CalPERS' TPA will report on the above measures according to NCQA technical specifications for the CalPERS-specific PPO population. CalPERS' PHM vendor will contribute to the results by providing the TPA with relevant data as needed. Both the TPA and the PHM will commit to put at-risk 22.5% of their total administrative service fee.
Going Beyond CalPERS – A Partnership to Improve Care for All Californians
CalPERS is engaging in this critical quality and equity work in close collaboration and alignment with its state purchasing partners: Covered California, which operates the health insurance marketplace under the Affordable Care Act, and California’s Department of Health Care Services (DHCS) which administers Medi-Cal, the Medicaid program in California. Together, CalPERS, Covered California and DHCS collectively provide health care to more than 18 million Californians, or 46% of the California population.
All three entities are also working with the Department of Managed Healthcare (DMHC) which regulates health plans covering 29.7 million lives in California. Covered California and DHCS, like CalPERS, require their health plans to report on the same measures found in the QAMS and each are attaching significant financial incentives to those measures. Additionally, DMHC is requiring all health plans it oversees to report on a limited measure set which includes all of the measures in the QAMS.
In addition, DMHC has also set a required benchmark and is requiring stratification by race and ethnicity to enable the identification of disparities. By aligning across purchasers and regulators on these critical quality and equity requirements, we hope to reduce reporting burden, put the spotlight on high-impact conditions that affect overall population health, eliminate disparities, and magnify the impact of our efforts to drive significant improvements in healthcare quality and outcomes for all Californians.